Prepared by Dr. Saeed Hassan
The article was published in “ACS Case Reviews in Surgery” on May 8, 2023. The authors who contributed to its writing are Maasher A, Hassan S, Yehya M, and AlDulaimi Q.
Simplified Summary for Patients and Laypeople:
This article discusses the case of a 49-year-old man who sustained multiple injuries after falling from a height. These injuries included a diaphragmatic hernia, which is a tear in the diaphragm (the muscle separating the chest from the abdomen). In this rare instance, a portion of the stomach moved into the sac surrounding the heart (pericardium), causing pressure on the heart. This condition is known as cardiac tamponade.
What Did the Doctors Do?
- Upon arrival at the emergency department, the man’s blood pressure was low (60/40 mm Hg).
- First, doctors inserted a nasogastric tube (NGT) to decompress the stomach and reduce the herniation, which eased pressure on the heart and improved blood pressure. Approximately 300 mL of gastric content was aspirated. This temporary measure helped stabilize the patient.
- After the patient’s condition stabilized and there was no internal bleeding, laparoscopic surgery was performed to repair the diaphragm defect. A nonabsorbable suture and a 10 x 15 cm composite mesh were used to close and reinforce the defect.
- The surgery was uneventful, and the patient recovered without complications. He was discharged on postoperative day 4.
Conclusion and Key Points:
- Traumatic intrapericardial diaphragmatic hernia is extremely rare, but it can be lethal if not diagnosed early and managed correctly.
- Inserting a nasogastric tube can temporarily resolve cardiac compression by the herniated stomach, stabilizing the patient before surgery.
- Laparoscopic intervention to repair the ruptured diaphragm is an acceptable option to minimize postoperative morbidities and shorten hospital stays, especially if adequate facilities and expert surgeons are available.
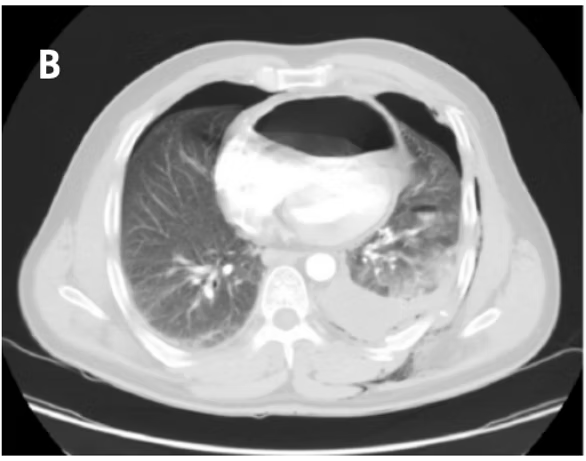
CT scan for traumatic diaphragmatic hernia, Dr Saeed Hassan
Read the full published article here
